See Your Best
Custom optometry solutions to enhance your vision For better performance at home, work, school, and play

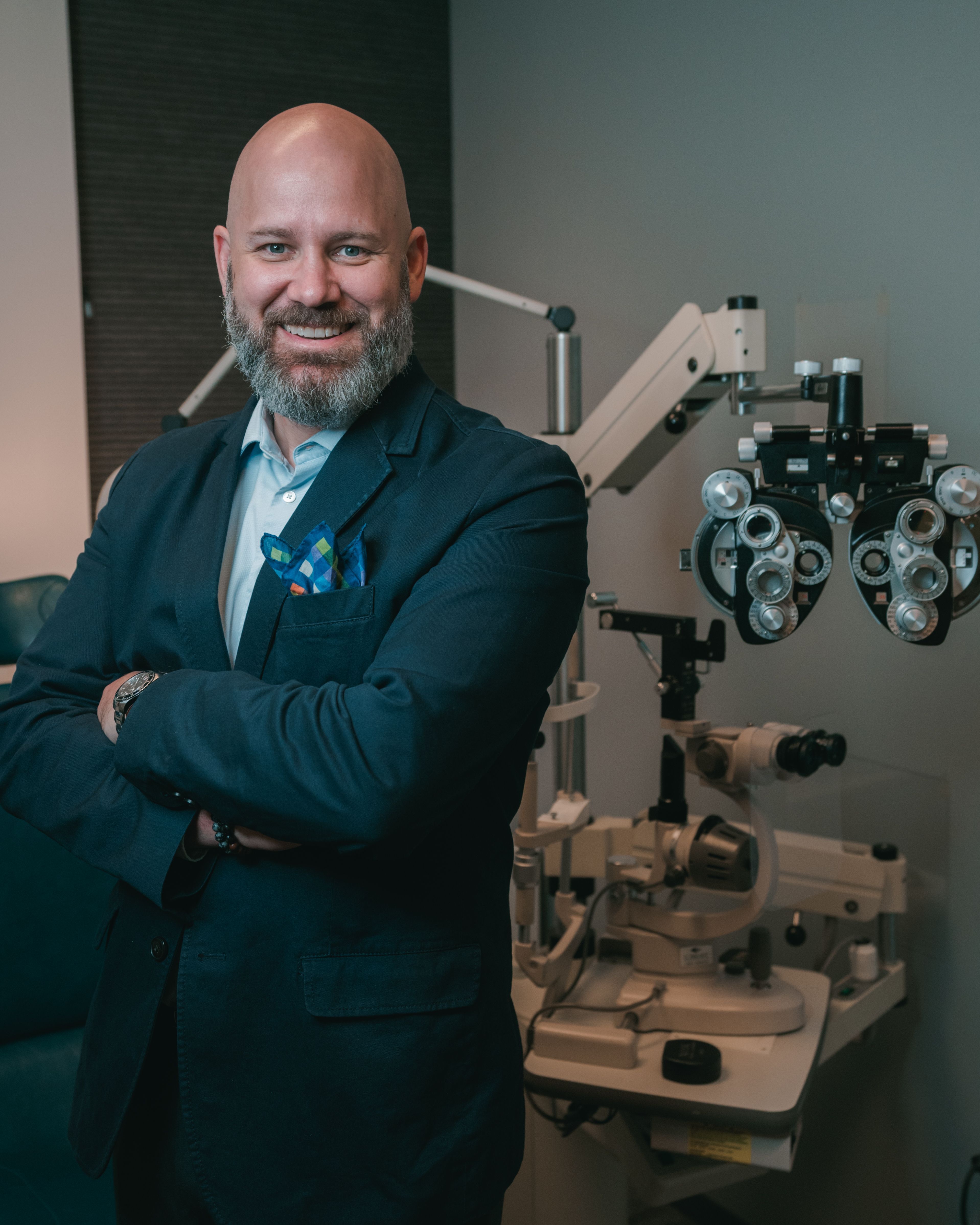
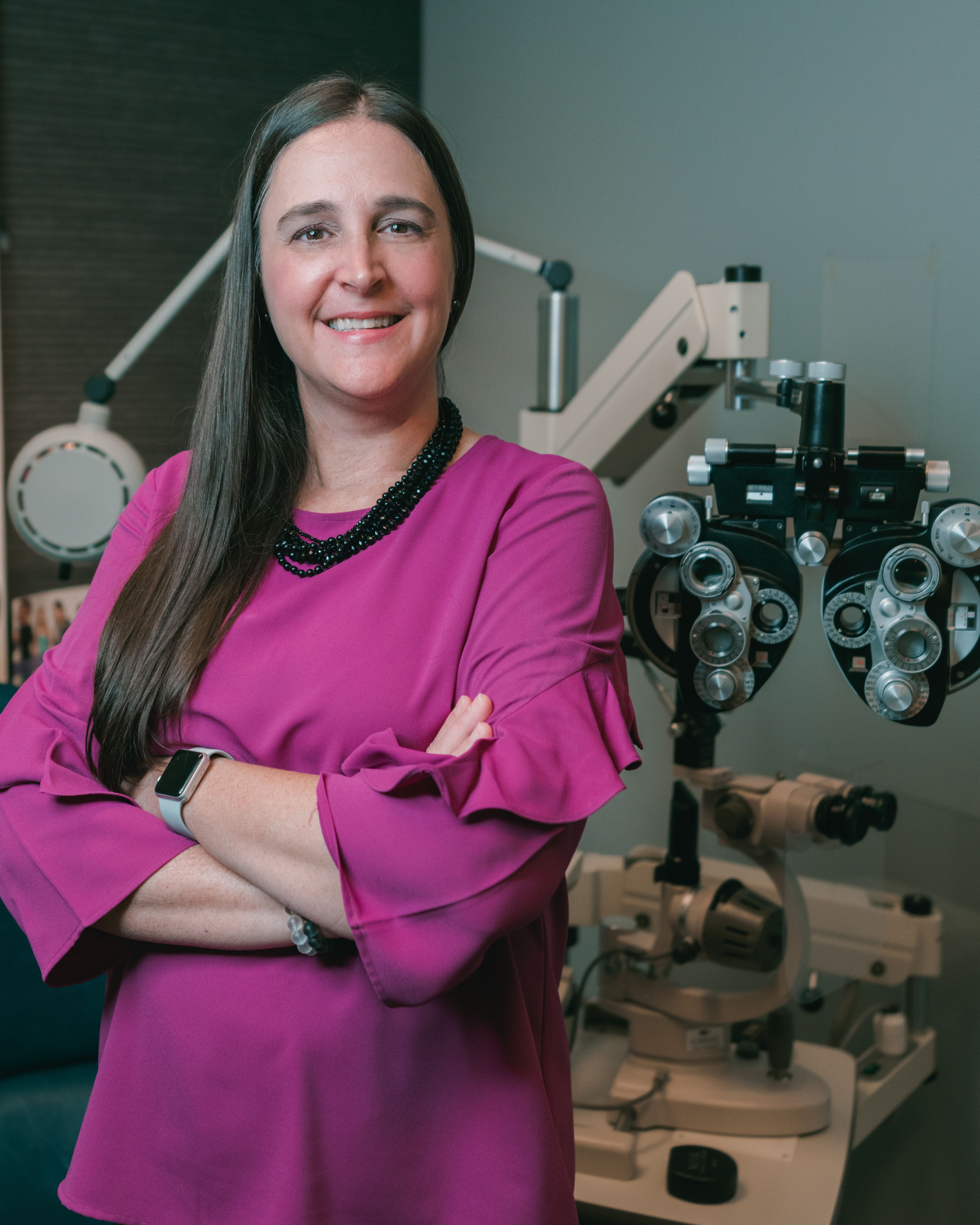
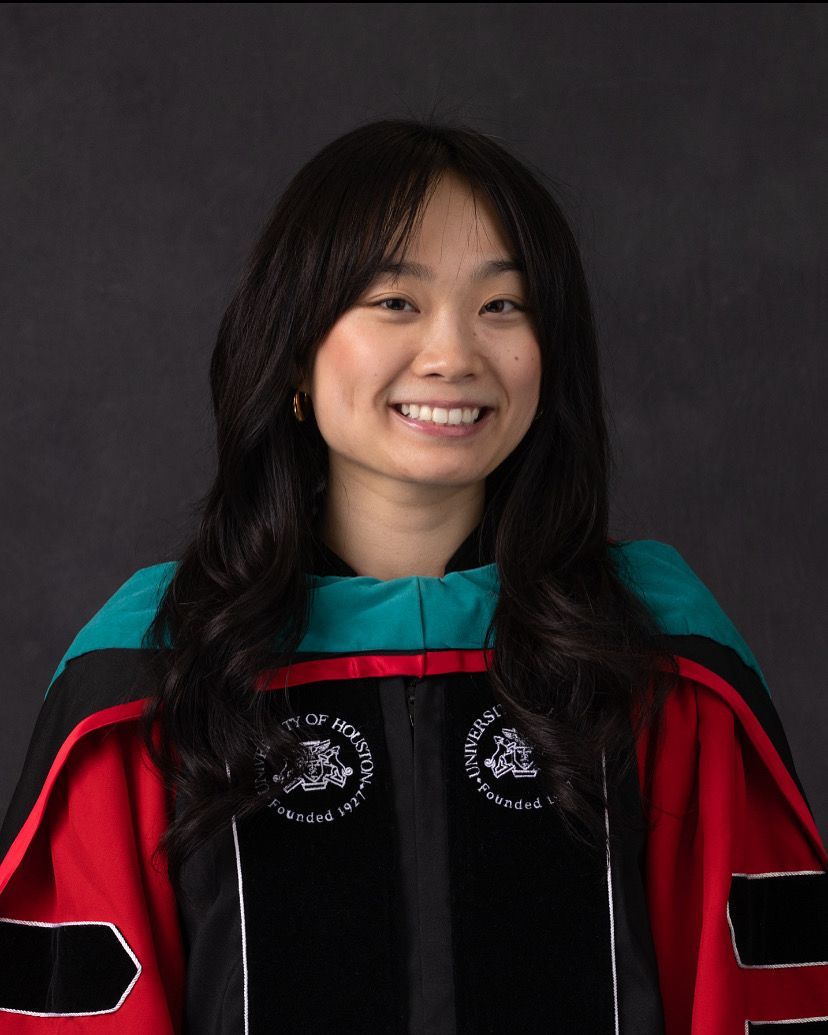
Welcome to Annandale EyeCare
We Care About You,
Our Patient
We are a dedicated team of eye care professionals with a singular focus of helping you see your
absolute best!
Since 1967 over 200,000 patients have trusted Annandale EyeCare to help them see their best.
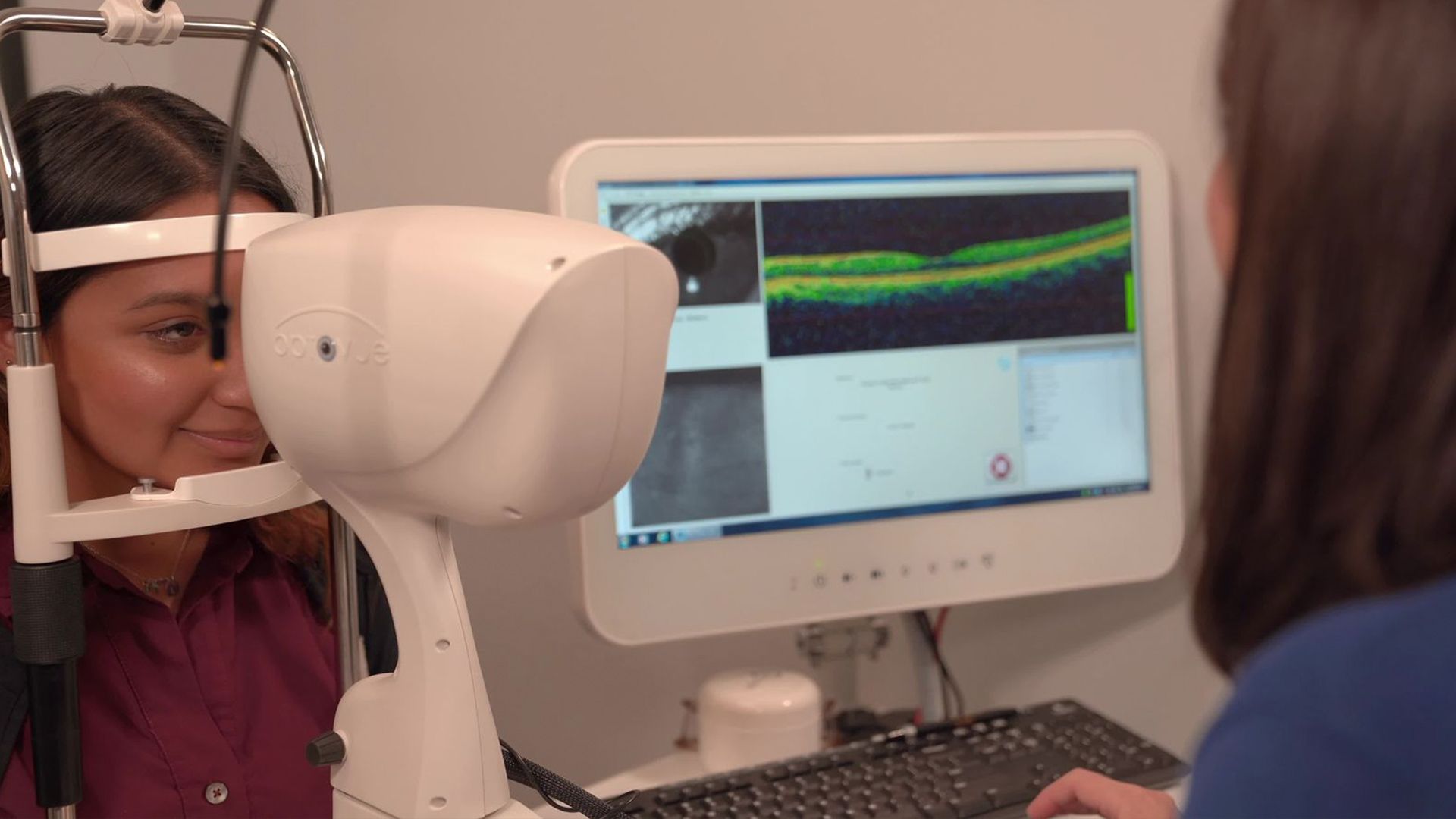
Featured Services
What We Offer
Pink Eye? Sudden Vision Loss?
Something In Your Eye?
Annandale EyeCare offers 24/7 on-call for eye emergencies. We are here for you!
We exclusively see established patients for after-hours emergencies.